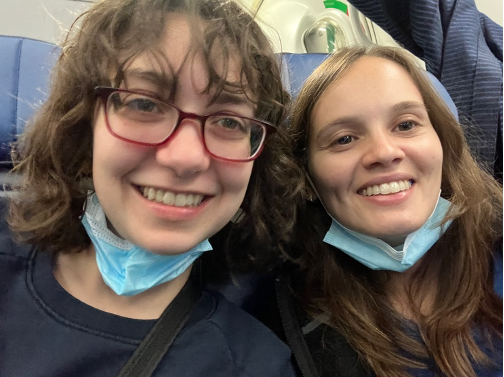
Maria Barra and Alexis Wilkinson traveled to Mozambique to perform research with the Richards-Kortum Lab. Their trip was funded by the Expanding Horizons Scholarship, generously provided by alumnus Walter Loewenstern.
Welcome to our blog post about our recent trip to Maputo, Mozambique! We are Maria Barra and Alexis Wilkinson, rising third-year Bioengineering Ph.D. students in the Richards-Kortum lab at Rice University. Through the Expanding Horizons fellowship funding, we were able to travel to Maputo, Mozambique in March 2023 to prepare a sample bank of cervical swab samples for evaluating novel HPV detection tests. Previously, we utilized the bank for test development and will continue to do so throughout our Ph.D. work.
Acknowledgments
We want to thank our advisor, Dr. Rebecca Richards-Kortum, for giving us the opportunity to travel to Mozambique to get a first-hand experience of the infrastructure and environment at Mavalane Central Hospital. We also want to thank the incredible doctors at MD Anderson Cancer Center, Dr. Kathleen Schmeler, Dr. Mila Salcedo and Dr. Ellen Baker, who have been working on providing screening and treatment to prevent cervical cancer in thousands of women for years. We also want to thank our collaborator in Mozambique, Dr. Hira Atif, without whom we would not have been able to get much done during this trip.
Relationship between HPV screening and cervical cancer
Human Papillomavirus (HPV) is a virus that is responsible for 95% of cervical cancer cases. If HPV infection is detected early, cervical cancer is extremely preventable. Therefore, it is important to catch HPV infection before it progresses to cervical cancer. In order to do this, HPV screening through DNA testing is recommended by the World Health Organization, and the most common method for doing this is called polymerase chain reaction (PCR).
What does our lab do?
Our lab develops low-cost diagnostic tests for use in low-resource settings, and one of our main focuses is HPV detection. PCR is very accurate and sensitive, but it is also an expensive and complex reaction that requires infrastructure and trained personnel that are usually unavailable in low-resource settings. This is why our lab strives to develop alternative methods to PCR that are appropriate for use in the sectors where they are most needed.

Why Mozambique?
Mozambique is a country on the east coast of sub-Saharan Africa and has one of the highest burdens of cervical cancer in the world. Cervical cancer is the most common cancer among women in Mozambique and, unlike in places with robust screening and treatment, the majority of women who develop cervical cancer die from the disease. Additionally, Mozambique is considered a low-income country ranking 184 of 187 on the Human Development Index. Unsurprisingly, there is a lack of infrastructure and resources for adequate HPV DNA screening and sufficient treatment. Since 2014, our collaborators at MD Anderson Cancer Center have been working with the Ministry of Health in Mozambique to implement HPV screening and treatment throughout the country.
Getting to Mozambique
Getting to Mozambique requires over 36 hours of travel. We first flew from Houston to New York, then to Johannesburg for an overnight layover, and finally, to Maputo the following day. We packed necessary lab supplies such as pipettes, Eppendorf tubes, and buffer which often raised some eyebrows while passing through security. We learned that having a letter from an authority figure at Rice helps moves things along more quickly. We strategically packed multiples of all the necessary supplies, both in checked bags and in our carry-ons, just in case any luggage got lost, which has happened frequently in past lab trips.

The sample bank
Through the programs implemented by the MD Anderson team, thousands of women have been screened for cervical cancer with a gold standard test. In order to do this, cervical swab samples are taken from patients and run on the gold standard test. The remaining sample is then labeled with a patient number and stored in the sample bank. We had previously traveled to Mozambique to evaluate an HPV test developed in our lab and ran into various issues when using the sample bank:
- Incorrect results in the sample database: for example, certain samples that were marked positive for a certain HPV type were actually not positive for that type
- Complete lack of organization made it impossible to find specific samples
- Hundreds of results reports of the gold standard test were not backed up and were lost. The information that was lost was crucial to understanding the functionality of our own tests.
The samples were stored in Ziploc bags, generally bigger than the one pictured below on the left, with no useful labeling. All of these bags were stored in the freezer at Mavalane Hospital, pictured on the right.
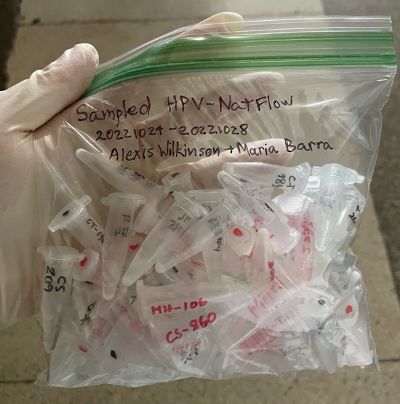

All of the issues mentioned above made it difficult to effectively evaluate our own test in development. Our goal on this trip was to organize the sample bank and prepare the samples stored there in order to be re-run on the gold standard test. This way we would be able to obtain and back up the reports of results from the gold standard test and easily find samples and their information for future use.
Working at Mavalane Hospital
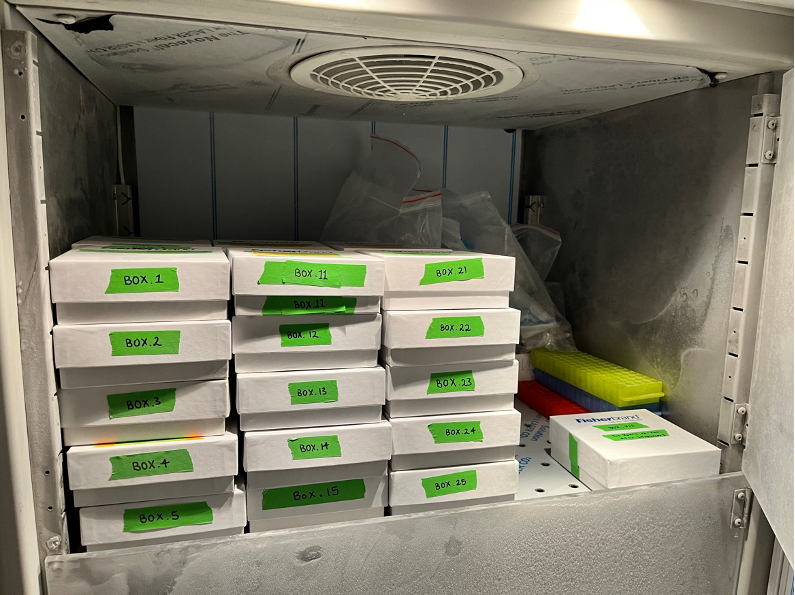
We worked in the building (pictured below) that houses the pathology lab at Mavalane Central Hospital. We mostly worked in the conference room where we organized samples into boxes, created Excel spreadsheets to keep track of them, and diluted them so they could be taken to a separate lab to be re-run on the gold standard test. We made sure to use PPE and disinfect the area at regular intervals to avoid contamination with clinical samples. We brought bottles of water from the hotel, not only for drinking, but also for diluting bleach and cleaning, since we had been told about water outages throughout the city. During one day, the hospital did not have running water – an unthinkable situation in the settings that we are used to. It was unsettling to think about the effects that this may have had on patients and our privilege to access water effortlessly have stayed with us since the trip.


Accomplishments
Within a week, we managed to organize over a thousand samples by HPV type into the boxes pictured below. The specific samples contained in each box are specified in the Excel sheets that we developed so they will be easy to find in future studies. We also successfully prepared over 500 samples to be re-run on the gold standard test and have compiled their respective reports with the results. They will then be uploaded to the database by another team member.
Reflections
The problems that we had encountered with the sample bank highlighted the need for a more streamlined and automated process to minimize errors and maximize organization amongst samples. How to implement this sustainably in the long-term in a low-resource setting is still unclear and something our team will consider for future projects.
Overall, this was an extremely productive trip for our lab. Our work will ensure that samples are accurately classified by HPV type and expedite future experiments on our tests in development. In large part, our success was due to our detail-oriented planning for the trip. We have previously noted that missing a single piece of equipment could mean significant setbacks in a resource-limited setting and planning with backups in mind is a must.
Lastly, we would like to thank the Expanding Horizons Fellowship for funding this trip that resulted in an optimally organized sample bank that will be extremely valuable to our lab and our specific PhD projects.
About the authors:
Maria is a 3rd year Ph.D. student in Bioengineering and is interested in global health and point-of-care diagnostics. Read more.
Alexis is a current Ph.D. student in Bioengineering. She is a rising third-year graduate student in the Richards-Kortum lab. Read more.
Further Reading:
Reflections on a summer of research in Costa Rica
Journey to Ecuador: Empowering Communities with Clean Water
Exploring the Unseen Strains – A Deep Dive into Research on Musician Injuries

